|
JULY
During the month of July I took the Advance Cardiac Life Support (ACLS) course which is required of all fourth year
med students. I asked to re-new my instructors license and after completing the course I was offered to take the ACLS instructors
course in October.
I also started to work on a computer presentation on how to remove a football helmet from an injured player which I hope
the emergency department and perhaps sports medicine will be able to use.
AUGUST
Trauma Surgery - Extremely busy since we have trauma coming into the ER 24/7. Saw a lot and I got to do a lot. We had
a patient who was a crane operator and had a 5,000 lb. beam crash through the cab of his crane and nearly squashed him like
a bug. I got to put in one of the three chest tubes he had put in due to "collapsed lungs" (pneumothorax) and blood in his
chest around his lungs (hemothorax). During the month I got to put in several more chest tubes, a central line (a big iv going
into the femoral vein), and a ton of suturing.
Also got to see, help, and learn how prepare a critically injured patient for the operating room once they get to the
ER. This was my main reason for doing trauma surgery since I know a trauma patients best chance for survival is getting into
the OR quickly.
SEPTEMBER
Emergency Medicine - Carolinas Medical Center
I'm currently doing an away month in Charlotte, North Carolina. Their Emergency Department is a bit bigger and busier
than UMC's. They see about 125,000 patients a year (compared to ~72,000 at UMC.) On my initial tour through the ED I noticed
they had rooms numbered from 1 through 115!! They also have their ED divided up into separate areas.
The Major Medical/Trauma area is where the seriously injured or sick patients go. These patients have a high probability
of being admitted. They have five trauma rooms where everyone puts on lead vest because they have overhead x-ray and are taking
x-rays as soon as they can get the patient positioned.
The Dignostic area is for those patients who don't seem to be quite as sick but are sicker than those who go to the Acute
Emergent Care area. The pregnant patient who is more than 20 weeks into her pregnancy and is having some type of complaint
would be an example of the patient seen here. I also took care of a patient complaining of abdominal pain. These patients
may need anything from emergent surgery to drinking Maalox or Pepto-Bismol and being told to start taking something like
Pepcid. So, the patients here may be admitted or may be sent home.
The Acute Emergent Care area is for those patients who probably will not be admitted but, need somthing more than a wound
check or suture removal which Fast Track is designed for. I've seen several women with sexually transmitted disease (doing
the PID shuffle for those in the know) and I've examined several people who came into the ED after they had a motor vehicle
crash earlier in the day. I also saw a patient with an abscess that did wind up going to the OR. So, you can't just assume
you will not get some patients that do need admitting. One of the residents was telling me that he had a patient complaing
of a severe toothache and the patient wound up having a full blown heart attack.
Fast Track is really designed to get patients in and out quickly. It's for those patients who need something simple like
a wound check following a laceration repair or to have sutures removed, etc. I thought Fast Track was open and we weren't
rotating through because it was staffed with Physician Assistants and Nurse Practitioners. I found out later that they
don't open Fast Track right now due to a staffing shortage. (Any nurses wanting to relocate should consider applying.)
They also have a Chest Pain center which can not only monitor the ECG of the patient but can constantly measure
the ST elevation. The ST segment is a part of the heart tracing that can show when the heart is not getting enough oxygen
and is starting to be injured. This can happen when a clot in one of the heart's arteries doesn't let as much blood flow through
as the heart needs.
They have two helicopter transport units (MedCenter Air) and, unlike UMC, they transport from the scene of an accident.
One of my first patients to take care of after MedCenter Air had transported him in, was a guy who was driving a riding
lawn mower to his neighbor's house to see if he could help him get the mower blade to start. En route, he got the blade to
start so he did a u-turn in the middle of the road and got T-boned by a car. First Responders told MedCenter Air's medics
that the lawn mower was destroyed and the rider was about 20 or 30 feet from point of impact. The guy was extremely lucky.
He was pretty much skinned up from head to toe and had a pretty big cut above and through his eye brow that the plastic surgeons
closed but, that was all. I just found out I was approved to do a ride along with Air Med for Monday, September 16. I'll try
to take some pictures and post them later.
Also, Charlotte reminds me a lot of Jackson, just a lot bigger!! It's cool seeing the hype and fan support for the local
NFL team (the Panthers) and of course NASCAR is big here since this is where Lowe's Motor Speedway is located. (As a
matter of fact, the exit for Lowe's Motor Speedway is not far from where I turn off going "home." I found out because the
first day I went North instead of South on my way to the hospital.)
The guy I'm staying with is originally from Jackson and he told me Charlotte had a lot of "small town atmosphere"
it was just spread out over a really big area.
Anyone who has an opportunity to do externship and rotate through CMC's hospital in Charlotte should take advantage of
the opportunity.
| MedCenter Air |

|
| I finally got to do a transfer in a helicopter. |
| Getting ready to land |

|
| We landed on the 50 yard line to pick up our patient |
| Ericson Stadium |

|
| Home of the Carolina Panthers |
October
This month I am doing an emergency medicine rotation at UMC. It is amazing how quickly time goes by when you are finally
doing what you dreamed of doing. I only have three shifts left in the ED at this time and it seems as if I just started.
Well, here are some of the moments that stand out during my month in the ED. I have had the opportunity to do many different
procedures during my M3 and M4 years. However, for one reason or another, I never had a chance to do a lumbar puncture (LP).
Finally, while in the ED at UMC, I had a chance to do my first LP. Unfortunately, my first two attempts were unsuccessful
and I had to let my resident take over. Now I am not implying that my overweight patient with scoliosis was too tough of a
challenge. It was however, a great deal easier on my third attempt which was on a thin, well muscular, male teenager. So,
I finally got my first LP.
I have also done a ton of laceration repairs and all of that suturing finally paid off. We had a patient come in with a
huge forehead lac that was bleeding extremely profusely. He had an altered mental status so we had to assume he had some kind
of head injury. Since direct pressure was not controlling the bleeding, I was told to close his lac by quickly suturing it
closed. I was told, "dont worry about making it pretty." Instead, I was told, "Just close it so he doesnt bleed out during
his CT scan." Well, trying to close a lac that is bleeding profusely, on a combative patient, is challenging to say the least.
With some help from one of the Air Care medics holding C-spine, I got the lac closed and he did well during his CT. Later,
with the help of some sedatives to keep the patient calm, we removed the initial sutures and closed the laceration properly
so there would be minimal scarring.
There was one difficult moment during the month however. Though I am not yet an emergency physician, I have worked with
many ED docs and most all have one thing in common. They can quickly assess a patient and spot those patients who are critically
sick and start the appropriate treatment. I found out that the attendings and residents at UMC are also well adept in making
these quick assessments. I had a patient come in with the complaint of, "I think I have the flu." They reported nausea, vomiting,
and all over body aches that started the previous day. Their biggest complaint was pain and kept rubbing their thighs during
the initial interview. There was no report of headache, stiff neck, photophobia, and there was no increase in pain with active
or passive movements. Their blood pressure was a little low, breathing was a little fast, but they were not tachycardic (heart
beating fast) and they did not have a fever. I suspected he had the flu along with dehydration. We started fluids and gave
Tylenol for pain and then we ordered labs. I was seeing another patient when I noticed the attending and resident was moving
the patient up front to one of the Major Trauma rooms. I went to see why and noticed that the patient had started breathing
even faster and was now tachycardic and very anxious. This was only about 30 minutes after I had seen them. Within an hour
of moving the patient up front, we were doing CPR, which was totally unexpected for someone who came in complaining of having
"the flu." We worked the code for over an hour. However, we were not successful in reviving the patient. Everyone was depressed
over the outcome and I think many were wondering what happened and what could we have done differently. Thankfully, the attendings
and residents follow up the patients us students see because they recognized much more quickly than I did, that this patient
was getting worse quickly. Later that same night, I got a call from the ED telling me the pathologist had a preliminary cause
of death as meningiococcemia. The meningiococcal bacterium usually causes meningitis, which is an inflammation of the layer
that covers the brain and spinal cord. Some people are carriers and are not affected by the bacteria. However, about 10% of
the time, it can become systemic and affect the entire body causing an overwhelming sepsis. I was taught in school that meningicoccemia
can be deadly when it goes systemic and a patient can die very quickly. However, there is a vast difference between reading
about how quickly a patient can die and seeing them die. To have a patient come in complaining of having the flu and then
having to code them within two hours certainly sticks with you. Since so many people were potentially exposed to this deadly
strain of bacteria, almost half of the ED had to return to the pharmacy so they could pick up some antibiotics to prevent
them from getting sick. It is frustrating when something like this happens. However, I do not think anything we could have
done would have made a difference since the patient deteriorated so quickly.
If I had any doubts about going into emergency medicine, those doubts have been dispelled this month. There is a constant
variety of patients coming into the ED. Some are simple and straightforward. Some start out as simple and become complex.
Like the lady who was complaining of her "gout" acting up. She did have gout but she also had her entire lower leg wrapped
in toilet paper. She said she scratched her leg on some barb wire A YEAR AGO! She had been taking care of it by pouring hydrogen
peroxide on the wound, wiping the wound with alcohol, soaking the wound in Epson salt, and covering the wound with petroleum
jelly prior to wrapping it with toilet paper. Her scratch now involved the entire lower leg with the infection spreading to
the bone.
Some start out complex and become more complex. Like the guy who came in with hemocromatosis (a genetic disease of the
liver in which the body takes in too much iron from food), cirrhosis of the liver, diabetes, congestive heart failure, heart
valve replacement, and impotence who was confused and complaining of not feeling right.
Some are prime examples of how some people do not consider the consequences of their actions. (I know some would call this
an example of stupidity however, I am trying to give them the benefit of doubt.) Like the guy who admitted to injecting heroin
into his forearms. He admitted to having open sores develop on both of his forearms, and he admitted to letting his pet parrot
perch on his forearms. Yes, believe it or not, he had huge infected sores on both of his forearms.
Anyway, it has been fun. It has been interesting, and I cannot wait to start my emergency medicine residency in July of
2003.
November
This month I am doing a sports medicine rotation. Last Friday (Nov.1), I was helping with a local high school football
team. Since they won, I will return tonight (Nov.8) to help cover their playoff game. Last Tuesday, I was on the sidelines
of Belhaven colleges mens soccer team. Soccer is one of those sports that are not done justice watching on television. Men's
soccer at the college level is very competitive and very physical. It does not quite have the same sound as standing on the
sidelines of a football game but, then again, the sounds you hear are not coming from pads and helmets hitting together. I
also helped Dr. Watts, the doctor I am working with this month, with a sports medicine lecture he gave to a group of physicians.
(I was the dummy, I mean patient, Dr. Watts demonstrated the exam techniques on.) The sales rep that sponsored the dinner
brought her husband along. I found out he was a pitcher for the World Series winning Anaheim Angels. I did not expect to be
eating dinner with a World Series athlete when I signed up for my rotation last year.
Anyway, the highlight of my rotation so far has been helping cover the S.E.C. womens soccer championship in Oxford at Ole
Miss. First, I can say I have finally been to Ole Miss. Now when someone sees me wearing my cap and asks me something about
"The Grove" or the stadium I will now at least have an idea of what they were talking about. Second, I can now say I have
been to a S.E.C. Womens Soccer Championship. As you can imagine, the players were pumped and ready for action. It is unfortunate
there were not more fans in the stands. I do not know if this was because the tournament started on a Thursday in the middle
of the day or if it was the distance the fans would have had to travel to their team play. Regardless if the girls were on
the winning or losing team, I believe they each gave 110% and they deserved a packed grand stand cheeering them on.
Some highlights from the first day of the S.E.C Soccer Championship. The number one seeded team (Auburn) was beat by the
number eight seeded team (LSU) in the first round of the tournament for the first time in S.E.C. history. There was one player
who landed badly and tore her ACL (i.e., she "blew her knee out") and one player was knocked unconscious when she received
a concussion. Naturally, I had to be for the home team and the Ole Miss players played hard. They scored earlier than any
other team that had played that day. Unfortunately, at the end of the game they were behind two to one. It was a very exciting
game to watch and I'm glad I was there.
I really lucked out being able to work with Dr. Watts this month. He not only works with Sports Medicine; he also works
with Family Medicine. If you think about it, having a primary care physician really incorporates an entire care package on
the field. Not just ortho injuries have to be taken care of. You have players with a history of diabetes, asthma, etc. that
may require medical assistance. Or, you may have a coach or spectator with a history of congestive heart failure, pulmonary
problems, or any other problem that affects the adult population. As far as ankle sprains, knee injuries, etc., an ortho doc
may have to be the one to ultimately treat or repair the injury. However, a primary care doc can just as easily recognize
that the player is injured and can start the required treatment to control pain and further injury.
Here are some links I have found for Sports Medicine if anyone is interested.
December
Sorry about the delay in updating what I have been up to. I spent December rotating through the Pediatric Emergency Department
(ED). I also started doing interviews as part of applying for my residency (more about this later.) Also, since the Pediatric
ED. works shifts like the adult side, I was able to spend some time with DGA, KT, and CC! (CC was home from North Carolina
for the holidays.) Oh yes, there was also the time spent fighting the crowds; stuck in traffic; and standing in line while
doing my Christmas shopping.
So, what is it like to work in the Pediatric ED? Well, I found out that kids get hurt in unique ways just like adults.
For example, one kid was standing up when the bus took off and he sat down abruptly onto a pencil. He was transported to
the Peds ED by ambulance while lying on his stomach. This was due to him having approximately four inches of a pencil imbedded
into the back of his thigh. Another kid was moving some metal behind his dads shop when a piece of metal that he was moving
slipped, hitting him in the face. However, his dad had another theory. He said that he had previously caught his son sword
fighting with his older son and he believes that he was hit in the face during their sword play. Anyway, the metal caught
him in the corner of his mouth and made a laceration about one inch long. On initial exam, it looked like he had cut all the
through his cheek to the inside of his mouth. Plastic surgery had to come in to close the laceration. Oh, by the way, remember
how your mom preached the evils of B.B. guns? Well, she was right. Kids are shot in the eye with B.B. guns.
Parents also do stupid stuff. Unfortunately, it is the children who usually pay for their parent's stupidity. Since U.M.C.
has the only Pediatric ED and Childrens Hospital in the state, many patients are transported to U.M.C. from all over the state.
During my rotation, I saw kids who were injured in car wrecks because they were not belted or properly restrained in a car
seat. I also saw one small infant who was seriously injured because the parent had placed the car seat on the front seat of
the car and did not have it facing towards the rear of the car. We also had patients who had drank/ate potentially poisonous
stuff like bleach; weight loss pills containing ephedra; and grandma's heart medicine. It still amazes me that some parents
simply do not believe anything can happen to their children and therefore do not see a need in protecting their children from
potentially dangerous situations.
I also found out that some parents will bring their kids to the ED for really minor reasons. More than once I told a parent,
Your child has a cold. Since most colds are caused by a virus (and no mom, anti-bacterial drugs, a.k.a. antibiotics, do not
help viral illnesses) we can only offer comfort care. However, there are times when a secondary infection can occur. For example,
when the membranes in the childs nose starts to swell and the child tries to blow their nose or they sneeze, they might force
bacteria into the ear canal that connects the ear and throat. This can cause an ear infection due to bacteria and we do have
antibiotics for ear infections. I also found out some parents will bring their child to the ED because they (the parent) want
a work excuse.
We also had the suspicious cases. One 18 month old was brought in because the parents were concerned he had hurt his leg
when he fell. The x-ray did show a fracture. But, it wasn't the type of fracture you would expect from a fall. Then, you notice
mom has what looks like an old black eye. The dad would not let the mom speak and he would never leave the room. We asked
one of the social workers to help us out since they have much more training in interview people about a delicate subject,
like possible child abuse, than I do.
We had another 16 year old come in after wrecking his four-wheeler. This in itself was not unusual. After all, the weekend
after Christmas we had four patients who were transported in after wrecking their A.T.V. (two with head injuries, none were
wearing a helmet). There were two patients transported after wrecking their bikes (one head injury, no helmets used) and we
had two trampoline accidents. Anyway, this guy said he ran from the accident site. (Ran from his own A.T.V.?) He said he hit
a tree, not a car. (Yet, the glass in his hair was the kind found in automobiles. After working on an ambulance for nine years,
you know what shattered safety glass looks like.) The uncle that brought him in acted like he was under the influence of
something (we found out later he wasn't the patient's uncle.) Anyway, before the patient was discharged we had to get campus
police involved to try and keep the peace since the uncle was telling us what he was and was not going to do. There is never
a dull moment in the ED, even on the pediatric side.
Technically, the Pediatric ED sees patients 16 years old and younger. But, some of these 14 and 15 year olds are bigger
than I am. (For that matter, I had an 8 year old boy who weighed 165 pounds.) Anyway, one of the pediatric residents was complaining
about one of his patients. His theory is that when they develop breast, pubic hair, and begin menstruating, they are no longer
a pediatric patient. Speaking of developing, I had several female patients come in complaining of lower abdominal pain. I
found out later, their abdominal pain improved immensely, once they found out they were not pregnant.
All in all, I had a really good experience in the Peds ED. As far as I know, the UMC Pediatric ED is the only place in
Mississippi you can go to 24 hours a day and have a board certified pediatric doctor and pediatric residents available to
treat your child. Needless to say, I learned a lot and I was able to brush up on examining and treating kids. I was also
able to do a couple of lumbar (spinal) taps which was interesting. And, I got to look in a million ears and dig out a ton
of ear wax! Woo Yoo!!
Now for an explanation of how residency works. First, consider that all medical students, regardless of what they will
eventually specialize in, take the same classes and do the same rotations during the first three years of school. The fourth
year of medical school, the student has their first opportunity to start taking some specialized classes. For example, my
classmates who are planning on going into pediatrics are taking as many pediatric rotations as possible. For those who are
going into surgery, they are taking a lot of surgery rotations.
Being able to work within a selected field gives you a chance to see if you are really going to enjoy specializing within
that field. It also gives you a chance to work with and meet some doctors who are already established within the field you
are planning on going into. This gives you an opportunity to get your letters of recommendation from someone who is (hopefully)
well known.
The reason all of this is important is because you have to apply for a residency position just like you had to apply for
medical school. Since I am planning on going into emergency medicine, I first had to decide which programs I would and would
not consider applying to for a residency position. I knew I did not want to move out of the southeast so, I did not even consider
applying to any of the other programs up north or on the East Coast or West Coast. Then, of the programs listed in the southeast,
I had to consider which ones I wanted to apply to for a position. For example, I did not apply to the Univ. Of Alabama at
Birmingham's program since it was just started last year and I am certain it probably has some kinks that need to be worked
out. I did not apply to some of the programs because of where they were located and I did not feel comfortable moving DGA
and KT into those areas. Others were ruled out because they did not see enough patients in their E.D. for me to feel comfortable
with the amount of hands on training that I would be receiving.
After you send off your application and it is forwarded to each program you listed, each program goes through the applications
and decides which candidates will be invited to interview with them. I will admit that I was a bit disappointed about not
getting back a ton of interview offers. On the other hand, Im glad I didn't spend several thousand dollars going all over
the southeast to interview when I already knew I was planning on ranking UMC as my number one choice.
When the students have finished interviewing, they will rank each place they interviewed in order of preference. Each
program will rank everyone they interviewed in their order of preference. Both lists go into a national computer bank and
the computer matches up each applicant with the schools. The idea is to try and give each applicant their preferred program
and at the same time, they try and give each program their preferred applicants.
In the best case scenario, each applicant will get either their first or second choice. If they don't get one of their
first two choices, then hopefully they will match with some other program they have listed. However, every year, there are
a few applicants that do not match with anyone on their list. When this happens, the national organization in charge of doing
the matching will contact the Dean of each school on the Monday of Match Week and give them a list of those applicants who
did not match into any of their requested programs. The Deans office will contact each student to let them know they did not
match. On Tuesday, all of the applicants that did not match (from all of the medical schools across the nation) will sit down
with a list of programs within their desired field that still have vacancies. They will basically be applying, interviewing,
and selecting a program within one or two days. Then, on Thursday, March 20th, senior medical students all across the nation
will open their letter and find out where they will be doing their residency.
Like I said, Im going to list UMC as my first choice because I hope to stay in Jackson. There are many more reasons for
me to stay in Jackson than there are for me to try and go elsewhere. UMC has the only Level I emergency department in the
state so they see a ton of cool stuff. They see over 70, 000 patients a year so I will get plenty of hands on training. Jackson
is only an hour and a half from home so it will be easy for DGA and KT to come home on the weekends if Im on call or working
a shift.
Oh, speaking of Jackson, I have been asked frequently where else in the state I can do my training. UMC is the only place
I can do my residency in emergency medicine. I have also been asked what is a residency. Think of residency as an advanced,
on-the-job training program where each year you will be given more and more responsibility and less and less supervision.
The first year graduates are known as interns. Even though they have the M.D. (Me Doctor) behind their name, they do not have
enough experience to function as a doctor independently and without supervision. Each intern will have all of the senior residents
(second year residents, third year residents, etc.) to help out and to ensure they don't overlook anything. And, all of the
residents have several attendings (Board Certified physicians within a particular field) looking over each of them.
Anyway, right now it is a bit strange. We don't know if we are going to stay in Jackson or move. DGA can't start applying
for a job until we find out where I am going to do my residency. If I do not stay in Jackson, then we will have from March
20th until July 1st to find someplace to live in whatever town I am going to do my residency in.
If I do match in Jackson, then I will hopefully, spend my first year as a newly graduated doctor (Post Graduate Year 1
a.k.a. PGY1), working in Internal Medicine. Then, starting in my PGY2 year, I will start focusing on my emergency medicine
training. Since my first year will (hopefully)be in Internal Medicine and then another three years will be spent in Emergency
Medicine, it will be four years from now before I am completely through with my training. (So, for anyone keeping track. I
spent four years re-taking my undergraduate/pre-med classes, four years in med school, and now I only have four more years
to go.)
As I said, right now we are in a kind of limbo. Were just waiting to see what develops and where we are going to move
to. Regardless if we stay in Jackson or move elsewhere, at least DGA and KT will be with me. (And CC, if she wants to leave
North Carolina ;)
JANUARY
January was a fantastic month for me. For one thing, I had an opportunity to do a research project in emergency medicine with
Dr. Summers. However, I was also able to spend a lot of time with my family. As a matter of fact, this was the most time I
have spent with DGA and KT since the summer between my first and second year of med school. For the first time in a long time,
I felt like I was a dad and husband again. When KT was sick, I was the one who picked her up from school. When DGA had to
work late, I was able to help out around the house. Anyway, as soon as I find out where I match for my residency, we can start
making plans to be together again. Living apart for four years has been a lot more stressful than I think any of us imagined.
As of now, DGA can't even start looking for another job since we don't know which town we will be in. Of course, we are hoping
to stay in Jackson (Ridgeland actually.) Anyway, we will find out on March 20. I'll try and keep everyone up to date.
Now, onto my research project. Last year when I was rotating at the VA hospital, I was reprimanded for bringing my cell
phone into the hospital. Later, one of the federal police officers working at the VA gave the wife of one of my patients a
written warning for using her cell phone within the hospital. This bothered me since I know the electromagnetic (radio) waves
a cell phone produces go in a straight line from the cell phone to the closest cell phone tower. The radio waves do not go
around a building. They go through the building. To satisfy my theory, I brought my scanner to the hospital the next time
I was on call. I was correct, I was able to pick up cell phone conversations on my scanner.
So, when Dr. Summers asked me if I had any ideas for a research project I told him I wanted to prove that cell phones
did not hamper our ability to monitor patients in the emergency department. After all, a portable cell phone only puts out
0.6 watts of power and the walkie-talkies that the Fire Department, E.M.S., and Police Departments use can put out up to 5.0
watts of power. The ambulances that I use
to work out of had a 100 watt amplifier in them. Also, the maintenance guys at U.M.C. go all over the hospital using their
walkie-talkies.
Personally, I think it is important to allow limited use of cell phones in the ED. If someones mother, father, child,
or other loved one is involved in an accident, then someone is going to be trying to find out the patients condition and pass
on the information to others. To not allow someone to use their cell phone and to force them to share a single pay phone with
a room full of people in the waiting room only adds more stress to a stressful situation.
So, Dr. Summers gave me an idea on how to go about proving or disproving my hypothesis. First, I did a literature search
to find out what research had already been done on cell phone use within the hospital. I found out that most of the research
that showed cell phones interfering with medical devices was done in the mid- to late-nineties. I also discovered that some
of the papers showing interference was based on the cell phones being operated within very close proximity or even touching
the medical device being interfered with. Of course, technology improves so quickly, I figured that the cell phones developed
today were less likely to cause interference. Then I found where the Federal Drug Administration had developed a test method
in late 2000 for cell phone companies to use to ensure cell phones do not interfere with the pacemakers or implanted defibrillators
that some people have. So, it seems that my thoughts about cell phone technology improving seems to be correct.
Next, I found a website that list every wireless antenna within the Jackson area. There are 55 antennas registered with
the FCC within the Jackson area. Four antennas are within two miles of U.M.C. Of course, all of the antennas are not cell
phone antennas. Some are for police, fire, and businesses like radio and television. My next step was to prove that the emergency
department was already being saturated with radio waves. So, I set up my scanner at different points and at different times
within the emergency department and made a list of the different cell phone frequencies I was able to pick up. The most surprising
discovery was when I set up my scanner in a supply closet that was located in the center of the department and directly behind
the x-ray department. Since, the x-ray department has to have shielded walls, I really didn't think I would be able to receive
very many frequencies. Instead, that was the location I picked up the second most number of frequencies. Granted, the conversations
werent all crystal clear but, I was still able to make out the conversations. (Oh, BTW, I was only able to listen to cell
phone conversations made on older analog phones. The newer digital phones transmit using 1's and 0's and each is transmitted
on a different frequency. I was able to hear the pulse burst of sound but, without a decoder, I could not listen to the conversations
made on a digital phone.) Therefore, I believe I was able to show that the emergency department is heavily saturated with
radio waves.
However, showing that the emergency department is saturated with radio waves also posed a new problem. What if someone
using a high power radio was using their radio outside and caused interference with my tests? So, to keep the potential interference
to a minimum, I conducted my experiment between 2 a.m. and 3 a.m. I had an EKG simulator hooked up to the EKG monitor in Trauma
room 2. It happened to work out that there was a patient on each side in Trauma rooms 1 and 3 who were also on an EKG monitor.
I used 3 different phones while standing beside the bed in Trauma 2, outside the door of Trauma 2 and standing by the monitors
at the nurses stations. I printed out EKG strips for each location with the phones turned on and with them turned off. I also
printed EKG strips while a police officer used his radio while standing in the hallway. I then mixed up the EKG strips and
asked different attendings, residents, nurses, flight medics, and an ACLS instructor if they could detect any interference
caused by the cell phones. There were a few EKGs that were questioned by a few however, the overwhelming majority agreed that
they could not tell of any interference caused by the cell phones.
Granted there are some deficiencies in my study. I could not test every cell phone in use. There are different EKG monitors
besides the ones used at UMC. Sprint PCS and Nextel transmit on different frequencies than the other cell phone companies
and I did not use a phone from either Sprint or Nextel.
As I said, January was a great month for me. I enjoyed spending time with my family. However, I also enjoyed the opportunity
to test a hypothesis that I had been thinking about. Who knows, maybe I'll have this or another research project published
one day.
| Wireless Towers in the Jackson Area |
|
FEBRUARY
I spent the month of February doing Internal Medicine (a.k.a. as "Medicine") at UMC. The difference between Internal
Medicine and Family Medicine is that the Family Medicine physician is trained to care for the entire family. In other words,
the Family Medicine physician is trained to: deliver babies; take care of infants and children; offer guidance and care during
the adolescent years; offer Ob/Gyn care; and to care for adults as they age. Internal Medicine is "adult medicine."
In other words, no babies, no children, and no Ob/Gyn. The Internal Medicine physicians spend three years focused on the diseases
of adults. Also, the specialists in adult medicine (Cardiology, Nephrology, Hematolgy, etc.) do an Internal Medicine residency
first and then they do additional focus training in whatever field they are going to specialize in.
So, what is the difference between an Internist and an Intern? An Internist is someone who specializes in Internal Medicine.
An Intern is someone who has just graduated from med school and is not eligible to take Step 3, which is the final test that
has to be taken to be a fully licensed physician. So, even though I will graduate from med school in May, I will be known
as an Intern for the first year of my residency. I will not have a state license and I will not have a D.E.A. number (i.e.,
I will not be able to write prescriptions for narcotics.)
Now for how my month went. SUPER! First of all, the Medicine service is responsible for the patients admitted to the hospital
with a medical problem (i.e., not surgical) and UMC admits some really sick patients. Since so many physicians have left the
state, the number of transfers to UMC has really increased. I had an opportunity to help take care of some really sick patients.
For example, we had patients with severe diabetic ketoacidosis, chronic pancreatitis, COPD exacerbation, worsening of congestive
heart failure, sickle cell pain crisis, really bad infections, and many other problems.
Another reason the month was a good month was because I had the opportunity to act like an Intern without all of the responsibilities
of an Intern. Granted, my months doing emergency medicine (adult and peds) allowed me to work as a resident, this month was
different. In the emergency departments, there is always an attending (a faculty member who is board certified within a certain
field) present. So, it is really neat if something bad happens because you have a "safety net" always close by.
However, in Internal Medicine the attending is usually present only during the mornings. There are always senior residents
around to help out if you get in a bind but, they are busy taking care of their own responsibilities. So, you are put in a
position where you are really acting on your on. Okay, not really. Since a fourth year medicine student can not sign orders
you are really limited in what you can do by yourself. But, you still have a lot of autonomy, which gives you the feeling
that you are "a doctor."
The final reason the month was awesome was because I was with two of the most efficient, well organized, motivated, and
knowledgeable residents I have every worked with. Michael acted with the confidence of someone that has already graduated
and has been practicing medicine for years. His ability to "get things done" was truly impressive. Josh was also
inspiring. He certainly did not act like an Intern who been a doctor for only six months. It was amazing how much information
he could recall on each patient. I was having a hard time keeping up with which test had or had not been done and what the
results of each test were. He certainly set a high standard for me to attempt to emulate during my intern year.
All in all, a super month and because of America's aging population (with their multiple medical problems), I have listed
Internal Medicine as my first choice for my transition year at UMC. (UMC's Emergency Medicine program requires you to do a
year of something else before you start your Emergency Medicine residency. In other words, they want you to finish the transition
from being a student to being a doctor before you start your training.)
All of the interviews are finished. All of the programs have been ranked in order of preference. Now all we have to do
is sit back and wait on Match Day to see where we will be.
MARCH
This month Im doing Family Medicine at Baptist Hospital. I'm basically doing the same thing I did last month but this time
we have children on our list of patients also. However, the most important thing about this month is the fact that we will
find out where I "Matched." I think I have mentioned before what the match is but, just in case I did not or, in
case you do not remember let me explain the process again. Basically, all medical students do the same thing the first three
years of med school. During your last year you get to customize your schedule so you can do rotations in the field you are
hoping to specialize in.
Applying for residency is just like applying for med school. You send out applications, you interview, and then you turn
in a list ranking your preference of every place you interviewed. Each residency program ranks everyone they have interviewed
and they turn in their list. The lists are matched up and almost all senior medical students (some programs matched early)
find out where they are going. Residency is the "on the job training" you get to help you hone your talents and
amass the knowledge you need for your chosen specialty.
So, from day one, all of my residents and attendings have been forced to listen to me count down the days to Match Day.
Speaking of residents, the Family Medicine residents are, in general, some of the happiest residents I have worked with. Since
Family Medicine is so broad and covers so much, their residents really have the opportunity to practice medicine in a number
of ways. Some will go into a traditional clinic setting where they will round on their patients who are admitted to the hospital.
Other will be content to working strictly Monday through Friday in a clinic without having to pull call at night or working
on the weekends. Of course, there will be others, like my senior resident this month, who will work in the emergency department.
I have pretty much decided that if I do not match into emergency medicine, I will probably do a family medicine residency
so I can work in the emergency department.
MATCH DAY
Well, for me, Match Day actually started three days early. The Monday before Match, any student who did not match to a program
they had listed would be notified that they have to "scramble." The scramble is exactly what it sounds like. If
you really want to do a particular specialty, and you do not match into that specialty, then you will have to get a list showing
which programs have vacancies. You then have to find a program that will take you before their remaining vacancies are filled.
The Monday before Match, I could not take the suspense any longer. I logged onto the website and saw, "Congratulations,
you have matched. I still did not know where I had matched. However, I knew I had matched in emergency medicine which was
a relief. For the last few years, there have only been single digit vacancies in emergency medicine after the match. So, I
was glad I did not have to try and locate a program elsewhere.
Now the only question that remained was, "Where will I be?" We were all hoping for UMC but, we would have to
wait until Match Day to find out. So, Thursday morning my classmates and our family and friends gathered in the Student Union
to nervously wait on our names to be called. Of course, there were the mandatory speeches by various people congratulating
us. Dr. Turner reported that 85% of the class got their first or second choice. 48% of my class will stay in Jackson with
the remaining 52% doing their residency elsewhere. My classmates will be doing residency programs in 28 states as far away
as California and Massachusetts. All of this was interesting and nice however, I'm thinking, "Lets go! I want to find
out."
We finally got started and our names were randomly called out. As each person had their name called, they deposited $5.00
into a black leather "doctor's bag" the bookstore had donated. The person who had their name called last got the
"bag of money." The bookstore had also donated other prizes. For example, the person who will move the farthest
away got a tee shirt with UMC's name on it. I was trying to keep from being too nervous by listing where my classmates were
going. All of a sudden, my name is called out. As I'm walking to the microphone to announce where I will do my residency I'm
scanning the paper for the results. My heart leaps to my throat as I read those magic words, Emergency Medicine - University
of Mississippi Medical Center - Jackson, Mississippi!!!!!!!!!!!!!!!!!!!!!!!!
Yes! DGA, KT, and I will be in Jackson for at least the next four years. This is absolutely the best thing that could
happen for us. I have no doubt I will receive fantastic training in emergency medicine. We will be close enough that we can
go home to visit on the weekends, even if it's for only a day. (DGA and KT can go home even if I'm on call or working on the
weekend.) Also, I doubt if KT is going to want to change schools in the 11th grade (the grade she will be in when I finish
my residency). So, being in Jackson will allow KT to graduate from a local school and still allow her family and friends from
home to participate in her graduation. DGA had to technically resign from her job so they could fill her position and have
someone trained before she left. DGA has not however, been able to send her resume out since she did not know where we would
be. The most important thing, is that DGA, KT, and I can finally start making some definite plans for us to live in the same
house again. It has been a lot more stressful living apart for four years than I think any of us imagined.
More Match Day Info
MEDICAL STUDENTS FIND THEIR 'MATCH' AT CEREMONY
Match Day 2003
During a Match Day 2003 program steeped in tradition, the Medical Centers 101 senior medical students discovered where
they would go for their specialty training.
The students matched to 20 different specialties: 58 percent matched in a primary care specialty; 48 percent will be staying
in Mississippi, while 52 percent will be going to residency programs in 21 other states.
Students matched to specialties "as diverse as anethesiology to urology," said Dr. Helen R. Turner, associate
dean for academic affairs and associate professor or medicine.
"You are certainly a diverse class with diverse interests and career goals," she said before the match results
were revealed. "Wherever you go, you will always be a part of the University of Mississippi School of Medicine. We are
proud of you, we wish you the best, and we know you will represent this institution to the best of your ability."
While addressing a Match Day audience for the last time as associate vice chancellor for health affairs and dean of the
School of Medicine, Dr. Wallace Conerly said he felt a particular attachment to the Class of 2003.
"It's been a delight to have all of you here these last four years," said Conerly, who will retire June 30.
"This being my last class to graduate, you are really special to me.
"I congratulate you on wherever you are going to go."
The match, conducted annually by the National Resident Matching Program (NRMP), is the primary system that matches applicants
to residency programs with available positions at teaching hospitals across the country. According to the NRMP, 14,332 medical
school seniors participated in the 2003 match, of which 93 percent were successfully matched to an open position in a participating
residency program.
Historically, at least 85 percent of seniors at UMC match with their first or second choices.
UMC's match results were revealed at 11 a.m. on Thursday, March 20 in the second-floor conference rooms of the Norman
C. Nelson Student Union. As Turner announced the names of each medical school senior in random order, the class members walked
to the front of the auditorium, placed five dollars into a medical bag, tore open the envelope that contained their matches,
announced their matches to the audience, and stuck colored pins into a large map to indicate their residency destinations.
The last student's name to be called - Marc Roy Lewin - received the medical bag full of money.
Turner challenged the students to realize that, although their medical education will continue with their newly announced
residencies, they will always be in a position to learn.
"As a physician, your education will never end," she said. "You must make a commitment to lifelong learning."
"As a group, you have studied together, had fun together and shared life-changing experiences. Through it all, you
have made lifelong friends."
In his closing remarks, Conerly urged the Class of 2003 to always remember two things.
"Leave the woodpile a little larger than you found it," he said. "And you've been taught how, so please
do deliver quality health care in a quality manner."
Bruce Coleman (3/31/03)
 CEREMONY ONE OF MANY 'ADVENTURES' FOR O'SULLIVANS
Match Day 2003
For most medical students, Match Day is an unforgettable exercise that ultimately determines not only the course of their
medical training, but their careers as well.
For Patrick Sean of Pascagougla and Jennifer Dance O'Sullivan, of Jackson, who each matched at UMC, the ceremony is just
another in two lifetimes of adventures.
Sean entered medical school to administer health care in the jungles of Asia; Jennifer to practice medicine in the heart
of Africa. The couple met one day in gross anatomy. One thing led to another, and the pair married during their third year
of medical school.
Now they are expecting their first child, a blessed event that had a profound impact on their residency decisions. Sean
chose family medicine and Jennifer selected pediatrics, primarily because "they are very family friendly residencies,"
Jennifer said.
"Neither residency staff dissuades you from having children, and they are very understanding," Patrick explained.
"We know the hospital, the floors, the computer system. If you want to do primary care, the challenges and the training
are comparatively the same here at UMC as anywhere else."
Then he offered an even more practical incentive: "Jennifer knew she didn't want to do surgery - she didn't want
to stand up on her feet for hours on end."
The ceremony of Match Day was embraced by the O'Sullivans, whose commitment to tradition may be best exemplified by their
absolute refusal to learn the sex of their child before it is born.
"You usually find out through an ultrasound at 20 weeks," Sean said. "We were in there for about an hour,
and I began to think we might as well find out. But Jennifer said 'No.'"
Once they've completed their residency training, the O'Sullivans can only hope their decision on where to practice will
be so cut and dried.
"During the interview process, we had to find out if the residency programs were open for us to do something overseas,"
Jennifer said. "Fortunately for us, both programs at UMC were.
"We have a lot of classmates who have already said they would be willing to come and arrange medical procedures for
us, so we look forward to the challenge - whether it be Africa, Asia or someplace else."
Bruce Coleman (3/31/03)
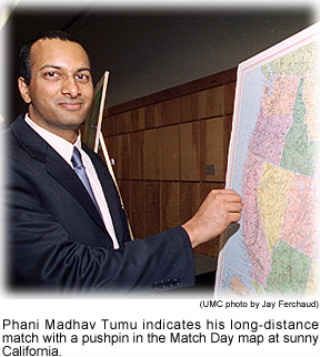 TUMU'S MATCH TWO TIME ZONES AWAY AT UCSF-EAST BAY
Match Day 2003
Phani Madhav Tumu is the early favorite to lead the UMC Class of 2003 in frequent flier miles.
He earned that distinction when he matched with the preliminary surgery program at the University of California at San
Francisco-East Bay - the furthest destination of Match Day 2003 participants.
Tumu said he has no reservations about leaving his parents in nearby Madison to continue his medical education two time
zones away. He has cousins in the San Francisco area. Although UCSF-East Bay wasn't his primary choice Tumu had no real preference
among the institutions he had listed for the match, he said the challenge of adapting to a new environment for his residency
is appealing.
"Mississippi is a slightly conservative state, and California is not exactly Republican," Tumu laughed. "But
San Francisco is a great place, and so many people want to live there.
"It's a great opportunity for me to go out to California and represent the state of Mississippi."
To help him do that, Match Day sponsors presented Tumu a T-shirt adorned with his home state - a little lagniappe for
having to go so far for his residency. But Tumu credits the education he received at UMC for paving the way for his residency
"Gold Rush."
"I actually feel very well prepared for this challenge," he said. "Residents and attending physicians allow
you to do so many things during your medical school training here, that when you go to other places, your skills stick out."
So when the California lifestyle becomes second nature to Tumu, will he be in danger of forgetting all about the Magnolia
state?
"Match Day is somewhat of a tradition that brings closure," he said, "but I haven't ruled out coming back
to Mississippi to practice."
Bruce Coleman (3/31/03)
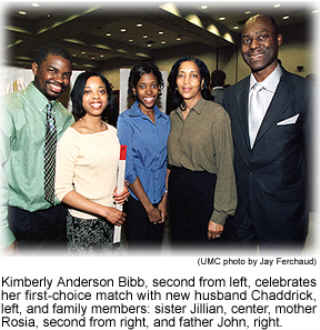 NEW MARRIAGE FIRM FOUNDATION FOR BIBB AT MATCH DAY
Match Day 2003
The home stretch of a medical school education specialty interviews and other demands may not seem to be the best time
to be a newlywed, but Kimberly Anderson Bibb's new marital status only enhanced her enjoyment of Match Day 2003.
Bibb's new husband, Chaddrick, celebrated along with his new in-laws when his bride announced she had matched with her
first choice, the family medicine program at the University of Alabama School of Medicine in Huntsville.
"The main thing that attracted me to that institution is that it is a university-affiliated with a community-based
setting," Bibb said. "Family medicine is the only program in that setting, so I'll be able to work with different
specialties one-on-one."
The couple also is pleased with the institution's location.
"It's only about five hours away from home," Bibb said. "Whenever I get homesick, I won't have too far
to go - both of our families are from Jackson."
Family ties are strengthened by personal milestones like Match Day, which not only determines the next phase of a medical
student's education, but also marks the accomplishment of a medical degree. Although Bibb enjoyed taking part in the tradition
of the ceremony, she suggested one aspect of Match Day she'd like to see altered a bit.
"It's kind of stressful opening up the envelope and announcing your match to the entire crowd of students, faculty
and family members," Bibb explained. "I would have preferred to open my letter individually with my family first,
then come to Match Day and announce it.
"But overall, I was well pleased with everything, and I thought the ceremony went very well."
Keeping an eye on the future, Bibb took time from the ceremony to anticipate the day she may return to Mississippi - not
to study, but to practice.
"I'm strongly considering coming back," she said. "This is my home, and I have a strong need to help provide
citizens of this state with quality health care.
"The training I received at UMC was excellent. My experience here is something I wouldn't have received elsewhere,
and I feel very competent and able to go into this residency and achieve my career goals."
Bruce Coleman (3/31/03)
|
